If You Throw, You Need A Different Kind of Rehab
Baseball and softball are growing in numbers and visibility in Ireland, especially at the recreational level. Injuries can and still do occur, but sports medicine is understandably built around hurling, Gaelic football and rugby. Throwing in baseball and softball is different. The forces are different. The long-term adaptations are different. Therefore the rehab has to be different too. If you throw, you need someone who understands throwers. Treating a thrower like a general shoulder is misguided.
Baseball and softball are growing in numbers and visibility in Ireland, especially at the recreational level. Injuries can and still do occur, but sports medicine is understandably built around hurling, Gaelic football and rugby. Throwing in baseball and softball is different. The forces are different. The long-term adaptations are different. Therefore the rehab has to be different too. If you throw, you need someone who understands throwers. Treating a thrower like a general shoulder is misguided.
The Hidden Forces of Throwing
Throwing a baseball is one of the most stressful movements in sport, especially for pitchers. At maximum layback, the elbow experiences roughly 60lbs of torque (the equivalent of five bowling balls pulling down on it). At ball release, the shoulder experiences a distractive force of about 1.2 times bodyweight, meaning the joint is resisting forces that are actively trying to pull it apart. All of this happens in less than a second, with the arm rotating at nearly 7,000° per second. These aren’t normal gym demands. Throwing places extreme stress on the shoulder and elbow at speeds and forces most rehab programs never prepare you for. Bands and light dumbbells might help early on, but if rehab never progresses to heavy strength work, eccentrics, plyometrics, medicine balls, and actual throwing, you’re not preparing for competitive throwing. If rehab doesn’t build you for the demands of throwing, it isn’t baseball rehab.
When Abnormal is Actually Normal
Because of the extreme forces involved in throwing, pitchers develop adaptations that don’t look “normal”, and they aren’t supposed to. The problem is that these adaptations are often treated as something to correct. A throwing shoulder is not a general population shoulder.
One of the best examples is humeral retroversion. After years of throwing, especially during youth development, the humerus gradually twists outward. This increases external rotation (ER) and decreases internal rotation (IR). This shift isn’t a flaw. More ER generally means more velocity. It also allows pitchers to achieve layback without over-stressing the front of the shoulder, because part of that motion is coming from bone structure and not just soft tissue laxity. But here’s where misunderstandings happen. A player presents with shoulder pain, IR looks limited, it gets labeled as GIRD (glenohumeral internal rotation deficit), and posterior capsule stretches are prescribed to “restore” the lost IR. Yet when both arms are measured properly, the total arc of motion in the throwing arm should be within about 5–10° of the non-throwing arm. If total arc is preserved, that “loss” of IR is just humeral retroversion — a normal and beneficial adaptation. Trying to aggressively correct that can mean altering the very adaptation that helps performance. This is why comparing a thrower’s shoulder to population norms can be misleading.
Labral findings are another example. Many throwers show labral changes on imaging due to the repetitive “peel-back mechanism” when throwing. However, many remain asymptomatic. Imaging findings alone do not equal dysfunction, especially in throwers. Treating the scan instead of the athlete is misguided. In throwers, the question isn’t “does this look normal?” It’s “is this functional and resilient for the demands of throwing?”
Asymmetry is a Feature, Not a Flaw
Baseball is inherently one-sided. You throw with one arm, you rotate in one direction, you load the same hip and shoulder, over and over again. The body adapts to this repeated stress - that’s the S.A.I.D. principle at work. Over time, throwers become structurally and functionally asymmetrical because the sport demands it. Rehab and strength training often aim for symmetry. Restoring baseline strength after injury is important but it’s in reference to the uninjured side. Perfect symmetry isn’t the goal in baseball; the goal is resilience within the asymmetry. A thrower doesn’t need to look balanced — they need to tolerate the demands of their position. In baseball, functional asymmetry is normal.
Return-to-Throwing is a Skill
Developing a return-to-throwing plan for a baseball or softball player is complex. Most interval throwing programs (ITPs) progress using distance (as a proxy for intensity) and number of throws (volume). This seems logical, but in reality, it’s far messier. Without wearable technology to measure elbow stress, or even a radar gun to monitor velocity, maintaining consistent intensity from session to session is difficult. Distance alone does not equal force as there is no perfectly linear relationship between how far you throw and how much stress is placed on the arm. Two pitchers who both throw 90mph do not necessarily place the same amount of stress on their arm either. Differences in mechanics, timing, strength, and body structure all change the equation. You can throw a short distance with maximal effort. You can throw farther with less effort. And that’s before we even introduce tools like weighted balls, long toss, and pulldowns. These methods may be effective for building arm strength and velocity because they intentionally increase stress on the system to drive adaptation, but they also alter mechanics and increase load. If used incorrectly or layered into a rehab process too early, they can easily set a player back.
Returning to throwing after injury is not just about being pain-free - it’s important but not the same as being ready to throw. Readiness requires: appropriate progression, controlled volume, gradual exposure to higher intensities, adequate recovery, and mechanical awareness. Returning to throwing is a matter of exposure to stress, and if you get the stress wrong, you can experience setbacks.
Specialized, Not Standard
If throwing creates unique adaptations, then our standards for assessment must reflect that. We cannot assess or rehab a thrower’s shoulder the same way we would a non-thrower’s. In general rehab, we often use the uninvolved side as the reference, but a thrower’s dominant arm should not look like their non-dominant arm or like the general population. Throwers often need greater ER strength, specific strength ratios that differ from standard “norms”, and unique endurance demands. If we apply generic shoulder strength standards to a thrower, we risk under-preparing them for the demands of throwing or over-correcting adaptations that are actually beneficial. A thrower’s shoulder isn’t broken because it doesn’t look symmetrical or textbook-normal; it’s specialized and specialized athletes require specialized assessment.
Protecting the Developing Arm
When we think about kids, we tend to imagine they’re indestructible — flexible, resilient, and able to bounce back from anything. Kids are just as susceptible to overuse injuries as adults, but the injuries look different. A common example is Little League Elbow (LLE). This is irritation of the growth plate on the inside of the elbow caused by repetitive throwing stress. In young athletes, the growth plate is the weak link in the arm. That’s why we don’t commonly see 10–14 year olds tearing their ulnar collateral ligament (UCL). The growth plate fails first. Once that plate closes (typically 15–17 years old) the weak link shifts and now the UCL becomes the structure at risk. The stress doesn’t change but rather the tissue that absorbs it does.
LLE is, at its core, an overuse injury and it reflects a broader issue in youth sports: early specialization and year-round competition. The baseball culture of today with travel teams, showcases, and constant exposure can quietly accumulate thousands of throws on a developing arm. This matters, especially when recovery, strength development, and overall athletic diversity are limited. Protecting young throwers isn’t about shutting them down. It’s about: managing throwing volume, respecting recovery, prioritizing long-term development over short-term exposure, and educating coaches and parents on how the throwing arm actually develops. Understanding the throwing shoulder and elbow isn’t just about rehab - it’s about prevention and giving young athletes the chance to keep playing for years to come.
Throwing is what makes baseball and softball unique and it’s also what makes players different to rehab. As the sports continue to grow in Ireland — in numbers, competition, and visibility — the need for informed, sport-specific injury management grows with them. Throwers cannot be assessed, progressed, or returned to play using generic shoulder guidelines. If you throw, you need someone who understands throwers. My role isn’t just to reduce your pain. It’s to understand the demands of your position, your schedule, and your long-term goals. It’s to manage load, guide progression, and prepare your arm for the realities of competition. It’s to return you to the field with confidence, not just clearance, because being pain-free isn’t the same as being ready.
How Dry Is Your Forest? Understanding Why Pain and Injuries Happen
When explaining why injuries occur, I often refer to the Biopsychosocial Model of pain (BPS). The BPS is a holistic model suggesting that health and well-being result from the interconnection and interaction between biological, psychological, and social factors, rather than a single cause.
When explaining why injuries occur, I often refer to the Biopsychosocial Model of pain (BPS). The BPS is a holistic model suggesting that health and well-being result from the interconnection and interaction between biological, psychological, and social factors, rather than a single cause.
But the BPS can be misunderstood by both patients and therapists. BPS doesn’t explain injury, but rather just considers multiple factors as opposed to specific causes. Some assume everything has to be perfectly balanced to remain injury-free. There are two problems with this: first, it’s impossible to have every aspect of life going perfectly at once, and second, it treats any single “off” factor as the cause of injury. One common argument against BPS is the incorrect interpretation that “it’s all in your head.” While this argument only factors in the psychological component, it’s generally meant that the physical factors, like movement, technique, biomechanics, and load, are ignored.
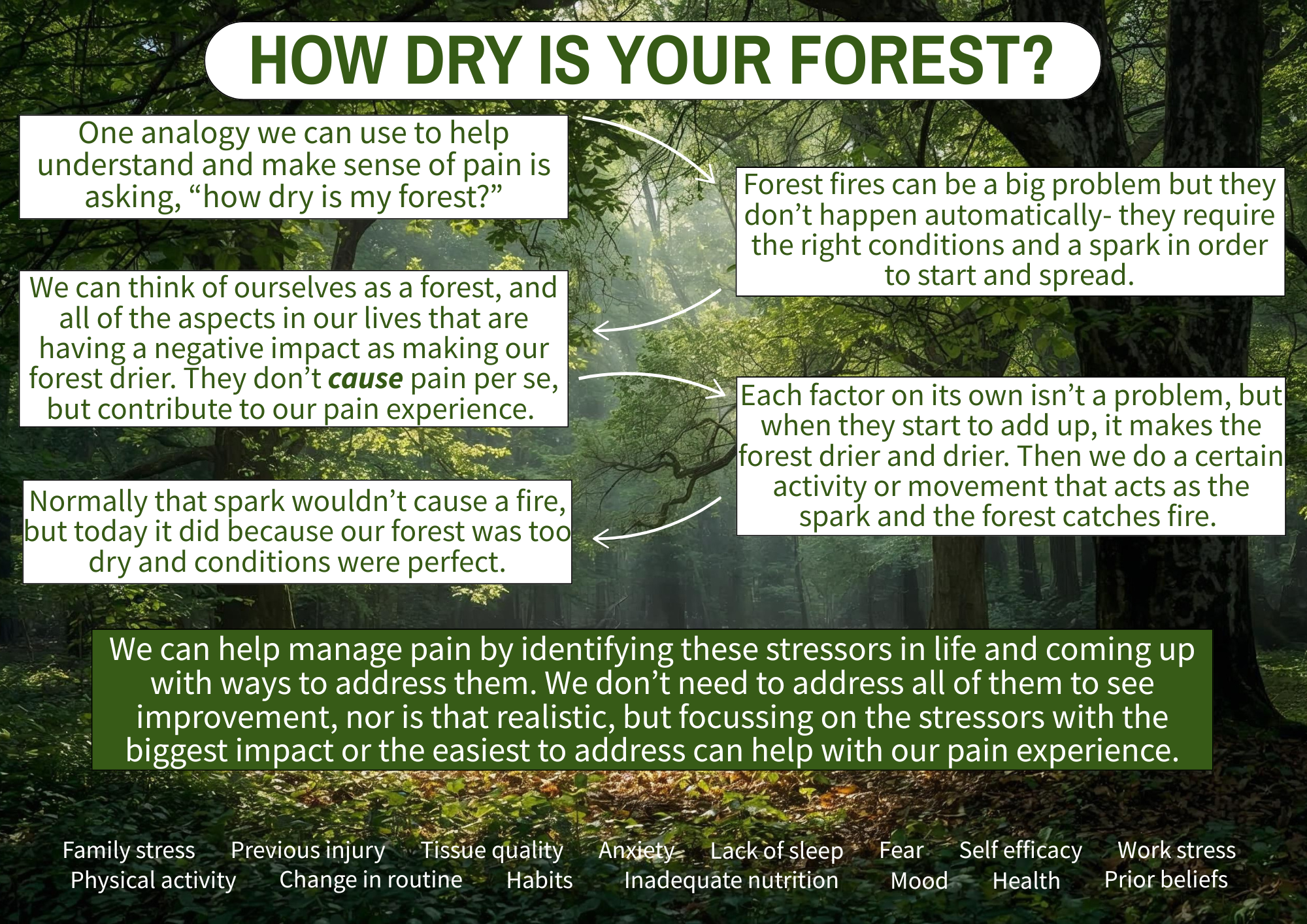
One analogy I really like that helps better explain BPS is asking yourself, “how dry is your forest?” This analogy comes from Ben Cormack, who suggests that many factors can make the forest dry, which then only requires a small spark to trigger a fire (i.e. pain). Greg Lehman has a similar analogy, asking how healthy is your ecosystem?
Think of yourself when you’re completely healthy as a nice, lush, green forest. Forest fires (pain and injury) are a problem, but they don’t occur automatically. Rather, they require the right conditions to start and spread. The factors under the three realms of the BPS can all individually make our forest drier; the degree to which they impact your forest will vary.
Biological factors include training volume, previous injury, nutrition, and sleep. Psychological factors include self-efficacy, confidence, mood, and anxiety. Social factors include work and family stress, habits, routines, and social support.
None of these factors cause pain, and each on its own is not a problem, but when they add up, they make our forest drier and drier. A lush forest would need a very big spark in order to start a fire, but a dry forest would only need a small spark.
This may explain the confusion people have when they feel they are doing everything right but still suffer an injury. “I only ran an extra 2km this week, and now my knee hurts.” In a lush forest, that 2km spark would not have been enough to start a fire, but in a dry forest, it was the perfect condition. Being stressed at work and not sleeping as well didn’t cause the pain, but they contributed to that 2km jump in training volume being more than what your body could tolerate.
The good news is that we don’t need to tackle all of the factors in order to see improvements in pain (nor is that realistic). Often, focusing on the stressors with the biggest impact or the easiest to change is enough. Taking the approach of “how can I be healthier” can also help as it will usually tackle several factors at once. But remember, these factors did not cause your injury but rather predisposed you or made an injury more likely. Sometimes the best course is to just acknowledge what has made our forest dry and to do our best to avoid a spark when our forest is dry.
The goal isn’t to find a single cause of pain. The goal is to understand what has dried out your forest, reduce a few key risk factors, and gradually rebuild capacity again.
What Managing My Own Knee Pain Has Reinforced About Rehab
Since I started running again almost a year ago, I’ve dealt with a few aches and pains. This most recent episode highlights a familiar situation for runners: staying active while still being smart with training.
Since I started running again almost a year ago, I’ve dealt with a few aches and pains. This most recent episode highlights a familiar situation for runners: staying active while still being smart with training.
Quick Summary
I had been consistent with my running into November, training four times a week with long, easy, and speed runs, while also lifting weights twice a week. During my first interval session of my program, I was exhausted early on and couldn’t complete the session. The following week, I noticed stiffness in my right knee when standing up from squatting while doing laundry, but I didn’t think much of it.
Over the next few weeks, travel and sickness disrupted my consistency. I still managed some runs, including an LSD PR of 13km, but during this run I noticed some lateral right knee pain. However, this didn’t affect my run and did not linger. Once I was back on track, I reorganized my plan to repeat a week, which led me to my 10km tempo run. At 4km I felt the same pain on my lateral knee and suddenly at 8km I was limping.
Even walking around the house, my knee was still hurting, but I still got outside for walks, trying to avoid hills as they were painful. About a week later, I attempted a run-walk to see if I could tolerate shorter runs interspersed with walking, but this was still immediately painful. Based on this, I decided to stop running until the pain improved. After doing some exercises and allowing the time, I ran the first kilometre of a 2km walk-run pain-free.
What the Heck is Going On?
Based on the location of the pain and how it worsened with bending and straightening my knee with running and walking, I would describe this as iliotibial band (ITB) related pain, a common running injury. The ITB is a thick, fibrous band of tissue formed by the gluteal muscles and inserting just below the knee. Its function is to increase the leverage of the gluteal muscles.
I don’t like calling this an “injury” as that implies damage to my knee, and there was no clear mechanism or event to suggest a tear. I feel it is more accurate to describe it as training errors leading to an overload and sensitization of my ITB causing pain.
Several factors in my training and life have led to this overload in my knee:
I didn’t sleep well or fuel myself enough prior to that first interval session, and I was stressed about an upcoming meeting later that day; all not ideal to then be going for an intense run.
Taking seven and 11 days off due to travel and sickness made my running volume inconsistent. While I hoped my capacity wouldn’t have dropped that much, running while sick was not ideal.
The strength training portion of my program also lacked consistency during this entire time. I didn’t necessarily get weaker, but it was still a break in training.
I jumped back in too quickly with a 10km tempo run despite slowing my pace. Although the distance was the same, it had been four weeks since my last tempo run.
What I am Doing to Manage
This became a red light situation for me, not because I was worried about damaging my knee, but because I knew based on the limping and lingering pain that running would only prolong this. I tried to compromise by doing the run-walk, but the immediate pain told me I needed a break until I could walk a significant time/distance (including hills) pain-free.
I chose to continue walking to stay active, trying to avoid hills and starting with slower and shorter walks. I also refocused on my strengthening, trying to find exercises that would be helpful. I started with some lateral hip and gluteal strengthening, which initially provided relief, but then focused on my quadriceps strength inspired by the pain with walking downhill. I chose Bulgarian split squats as my main exercise as I could load in a single-leg and bent knee position. My knee improved once I significantly increased the weight after the initial painful phase. I also added some hopping to re-accustom myself to the single leg loading of running.
Just last weekend, I went for a walk-run, opting to start with walking to get warmed up and stuck to a distance, even if it went well. The first kilometre of running was pain-free, but the second had some pain, though manageable. I plan to continue running as the pain is down to a yellow light, ensuring I continue to improve before restarting continuous running.
Even as an athletic therapist, I am still active myself. I started running again with walk-runs last January after 14 years, only to end up back at them and having to build myself back up. Like many setbacks though, the silver lining is the opportunity to reflect, evaluate your program, make changes, and learn from your mistakes. I now know for the future that even taking just a week or two off requires some adjustments to my running volume. I don’t feel this current pain was caused by running mechanics or lack of strength. While these factors are often cited as causes, they ignore all of the other factors that lower capacity and/or increase load. I don’t feel any single factor was the cause— they all contributed to create the ideal conditions for ITB-related pain.
To Summarize
My ITB-related knee pain developed due to various factors, forming the perfect storm.
This is not an injury, but pain due to overload and training errors.
Several internal factors and a jump in interval volume likely triggered the knee sensitivity.
I had gaps in my running and strengthening consistency, further lowering my capacity.
I had two load spikes that were more than I could tolerate, resulting in the ITB pain.
I remained active with walking despite some pain, and added strengthening exercises specific for my knee.
I will continue to progress my walk-runs to continuous running, using pain both during and after to guide my progress.
Pain rarely comes down to one thing, and rehab rarely follows a straight line. What matters more than finding the “cause” is having a way to make decisions as symptoms change. This is the same framework I use with clients — not because it guarantees a perfect outcome, but because it gives us a clear way to adapt, stay active where possible, and keep moving forward even when things don’t go to plan.
My Five Guiding Principles
Since becoming a certified athletic therapist in 2017, my approach to sport injury rehab has evolved. Like many therapists, I initially followed my school teachings, but over time, I’ve learned from my experiences, colleagues, and continuing education. I’ve identified what resonates with me, guides me, and works best for me. I’ve ‘found my flow,’ as described in school.
Since becoming a certified athletic therapist in 2017, my approach to sport injury rehab has evolved. Like many therapists, I initially followed my school teachings, but over time, I’ve learned from my experiences, colleagues, and continuing education. I’ve identified what resonates with me, guides me, and works best for me. I’ve ‘found my flow,’ as described in school.
While I aim to continuously learn and adapt, there are five principles that I believe are not only foundational to me but are likely to remain constant.
The Body is Adaptable
I think at the forefront is the idea that the body is adaptable. We know this occurs because we have concepts like Wolff’s Law (which describes how bones remodel to load), Davis’s Law (same as Wolff’s but for muscles, tendons, ligaments, etc…) and the SAID principle (specific adaptations to imposed demands- we get better at what we practice). A perfect example of this is when we workout at the gym and we do bicep curls (with progressive weight and adequate recovery), our biceps get bigger. When we stop working out, our biceps get smaller. But guess what- we can make them big again by doing curls again.
Our body can change and it responds to the loads and forces that we place (or don’t place) upon it. Obviously I like to focus on the good, but certainly if we train really hard, don’t allow for adequate recovery and experience injuries, we’re going to have a negative adaptation, ie injury. A lot of people may refer to this as “wear and tear” as if we’re a machine, but when we apply the right load and recovery throughout our training, it becomes “wear and repair”.
Load Drives Recovery
To piggyback on our adaptability, it all comes down to appropriate loads on the body, and this drives recovery from injury. Our body needs a mechanical or physical stimulus regularly and progressively in order to drive these adaptations if we want to get back to our sports and reduce our risk of reinjury. We need to prepare our body again for the demands it is going to face in our sport.
Rehab Should Be Active, Not Passive
Rest and passive treatments do play a role the role of pain management in our recovery process, but this should only be within the first few days (ie the inflammation stage of healing) and should wane and give way to progressive exercises. The problem with passive treatment is two-fold: it doesn’t load and prepare the body for physical activity, and it can make patients dependent on their therapist to get them better. Patients have better results when they are active in their recovery, literally and figuratively.
Education First
If you don’t know what you’re dealing with, how can you expect to manage it? The British physiotherapist Louis Gifford believed that patients want to know four things:
“What’s wrong with me?” They want to have an accurate diagnosis.
“How long is it going to take to get better?” Having a prognosis can help them plan their future.
“Is there anything I can do to help get better?” They want some self-management techniques.
“What can you do to help me?” This can include any number of things to help you feel better.
If I can provide an accurate diagnosis and explanation for someone’s injury, provide a timeline and idea for what recovery is going to look like, give them ways to help their own symptoms and provide a plan for a fully recovery, I am going to do a lot to help them with any anxiety and fears and help them take control and empower them throughout the process.
Resilience is the Goal
Ultimately, resiliency (the ability to adapt to stress and bounce back) is the goal. A patient should not feel broken or something is wrong with their body whenever they come into an appointment. They should not feel like they have to come in regularly in order to continue their sport. They should feel strong and confident in their body to compete after an injury. They should feel they were active and driving the recovery, and that if something does come up, they have the tools and resources to manage without feeling like they’re broken again.
Making Virtual Rehab Work For You
Some people may still be on the fence about virtual athletic therapy, even knowing it can be just as effective as in-person care. While virtual care has its limitations, there are simple ways we can address them and make the experience more personal, effective, and rewarding.
Some people may still be on the fence about virtual athletic therapy, even knowing it can be just as effective as in-person care. While virtual care has its limitations, there are simple ways we can address them and make the experience more personal, effective, and rewarding.
The virtual element
It is understandable that some patients feel more comfortable talking about their pain and injuries face-to-face with a practitioner as there is that physical interaction. Talking through a computer screen may feel distant, cold, and ineffective at first, but they get easier with consistency and practice. It is still possible to build trust and alliance through a screen, and this can be done with clear communication and open conversation. As well, making sure you are in a well-lit and open space and in comfortable clothing to move can help the session feel more natural. The first session might feel awkward, but by the second or third, it starts to feel familiar.
No hands-on assessment
There is no denying that physical touch is an important part of in-person rehab as touch can have many direct and indirect benefits during assessment and treatment. But much of what we learn through hands-on testing can still be gathered virtually. Guided movement tests and a clear history provide just as much insight into your pain and limitations. Many of the traditional “special tests” used in clinics don’t always have great accuracy anyway, so what really matters is understanding how you move and what you feel. A lot of valuable information can be gathered through an open and honest conversation to make an accurate assessment.
No hands-on treatment
Much like assessment, physical touch and rehab treatments are thought of going hand in hand (no pun intended). Patients expect, when coming into a treatment session, to be massaged, rubbed, stretched, or cued through exercises. They often expect something to be done to them, whereas virtual care focuses on what they can do. Without the physical interaction, the treatment shifts to self-management strategies and exercises for the patient to do on their own for long-term improvement.
Technology isn’t always perfect
Technology has a habit of acting up at the worst times. Some simple steps prior to the appointment to ensure an enjoyable experience include making sure you have an adequate internet connection and that your device’s speakers and microphone work can help ensure the call quality is optimal. There will also be a plan in place with instructions prior to the appointment should the session be interrupted.
Not suitable for every condition
Some conditions will always benefit more from in-person care, but others can be managed surprisingly well online. In the study (Lawford et al., 2018), some participants noted being skeptical at first of receiving care for their knee osteoarthritis via telephone appointments, but later embraced it. Others (Fraser et al., 2019) thought themselves unsuitable for virtual care but were still willing to try. This is to say that there is no harm in setting up a consultation to ask questions about your suitability for virtual care.
Perception of Inferiority
Overall, many patients may feel that virtual care is inferior to in-person due to the lack of physical interaction and hands-on contact. They may feel that education, advice, reassurance, and exercise prescription are not enough. A shift in mindset and embracing self-management may be needed, but this is not easy to overcome and will take time. It is important to remember that the quality of care isn’t defined by the format, but by the communication, planning, and consistency of a rehab treatment.
Some people will always prefer in-person care — and that’s completely fine. Virtual care isn’t here to replace it, but to make rehab more accessible, flexible, and practical. What matters most is that you find a therapist you trust and a plan that fits your life. If you’ve felt stuck with in-person appointments, virtual care might be the change that helps you move forward.
References:
Fraser C, Beasley M, Macfarlane G, Lovell K. Telephone cognitive behavioural therapy to prevent the development of chronic widespread pain: a qualitative study of patient perspectives and treatment acceptability. BMC Musculoskelet Disord. 2019; 20 (1):198-1008. doi: 10.1186/s12891-019-2584-2.
Lawford BJ, Delany C, Bennell KL, Hinman RS. "I was really sceptical...But it worked really well": a qualitative study of patient perceptions of telephone-delivered exercise therapy by physiotherapists for people with knee osteoarthritis. Osteoarthritis Cartilage. 2018; 26 (6):741-750. doi: 10.1016/j.joca.2018.02.909.
Virtual Care: What It Can’t Do (And Why That’s Okay)
While research shows virtual rehabilitation can be as effective as in-person care, it’s important to recognize that it isn’t perfect. Understanding its limitations helps patients make informed choices and know what to expect before starting virtual care.
While research shows virtual rehabilitation can be as effective as in-person care, it’s important to recognize that it isn’t perfect. Understanding its limitations helps patients make informed choices and know what to expect before starting virtual care.
Lack of Physical Interaction
One of the most common themes in the research evaluating virtual care is how patients view the physical aspect of injury assessment and treatment. Obviously, physical interaction is not there with virtual care, which many patients felt affected their ability to develop rapport with their therapists, leading to an impersonal relationship. Some people feel more natural and personable when they are face-to-face with a therapist as they can get a better sense of tone and body language. It can be hard for some to replicate casual conversation through a computer screen and therefore may find it harder to build that connection and trust.
Lack of Physical Contact
Understandably, many patients feel a big part of the injury rehabilitation is the physical touch aspect. Physical touch is used in many ways during assessment, such as to test range of motion and strength, feel for muscle tone and tenderness, see swelling and movement tests, or even just to provide comfort and reassurance. As well, many people value the physical contact during treatments through either manual therapy or assistance with exercises. While manual therapy is not the main driver of recovery, it can play an important role in calming symptoms, relieving stress, restoring comfort, and building confidence in movement, all things that can make a difference early in rehab.
Perception of Inferiority
Because of the lack of physical interaction and touch, some patients may feel virtual care is inferior to in-person care. Some patients have noted not feeling confident in the therapist’s assessment because of this lack of touch, and may feel that advice, education, and guided exercises are not adequate enough. This can have an impact on motivation and expectations, which affect the outcomes of treatment.
Not Suitable for Every Condition
While virtual care is suitable for many of the common musculoskeletal conditions, it does not work well for all. Post-operative patients usually require early and consistent mobilization— while this can certainly be guided virtually, having that physical touch and leverage can help patients push a bit further than they might on their own. When it comes to return-to-play decisions, having valuable objective measures like equal range of motion, strength, and power can make better informed decisions. Certain symptoms like numbness or loss of strength may require a more thorough neurological exam that is better done in person. Patients may even feel safer when completing exercises by having someone beside them to guide or adjust movements or even motivate them. These are examples where in-person care may be more beneficial, but virtual care can still play a role in determining what’s appropriate and in helping guide recovery.
Technology Isn’t Always Perfect
Current technology is amazing, but it is not always easy to use or reliable. Bad internet connection leading to audio and visual lagging or poor lighting and camera angles can make an appointment frustrating and a less than ideal experience. Comfort and technology literacy can be an issue too, as some patients may not feel confident doing video calls or using the programs/websites that provide their home exercise program. Some patients may even have concerns regarding the safety, privacy, or confidentiality of online video calls. While the programs that Bend Without Breaking use are GDPR-compliant, these are still valid and understandable concerns.
Some patients in the literature reported being sceptical of virtual care at first but later embraced it. Still, virtual care isn’t for everyone — and that’s okay. Some people simply prefer the structure, environment, and physical interaction of in-person care. What matters most is that your treatment feels valuable and effective for you. Virtual care isn’t here to replace in-person care, but to make quality rehab more accessible, practical, and convenient.
References:
Barton, C. J., Ezzat, A. M., Merolli, M., Williams, C. M., Haines, T., Mehta, N., et al. “It's second best”: A mixed-methods evaluation of the experiences and attitudes of people with musculoskeletal pain towards physiotherapist delivered telehealth during the COVID-19 pandemic. Musculoskeletal Science and Practice. 2022; 58, Article 102500. https://doi.org/10.1016/j.msksp.2021.102500.
Bennell KL, Marshall CJ, Dobson F, Kasza J, Lonsdale C, Hinman RS. Does a web-based exercise programming system improve home exercise adherence for people with musculoskeletal conditions?: A randomized controlled trial. Am J Phys Med Rehabil. 2019; 98 (10): 850-858. doi: 10.1097/PHM.0000000000001204.
Bucki FM, Clay MB, Tobiczyk H, Green BN. Scoping review of telehealth for musculoskeletal disorders: applications for the COVID-19 pandemic. J Manipulative Physiol Ther. 2021; 44 (7): 558-565. doi: 10.1016/j.jmpt.2021.12.003.
Cottrell MA, Galea OA, O’Leary SP, Hill AJ, Russell TG. Real-time telerehabilitation for the treatment of musculoskeletal conditions is effective and comparable to standard practice: a systematic review and meta-analysis. Clin Rehab. 2017; 31 (5): 625-638. doi: 10.1177/0269215516645148.
Cottrell MA, O’Leary SP, Raymer M, Hill AJ, Comans T, Russell TG. Does telerehabilitation result in inferior clinical outcomes compared with in-person care for the management of chronic MSK spinal conditions in the tertiary hospital setting? J Telemed Telecare. 2021; 27 (7): 444-452. doi: 10.1177/1357633X19887265.
Cottrell MA, Russell TG. Telehealth for musculoskeletal physiotherapy. Musculoskelet Sci Pract. 2020 ;48: Article 102193. doi: 10.1016/j.msksp.2020.102193.
Cronström A, Sjödahl Hammarlund C. "A feeling of being part of the future": a qualitative study on physical therapists' experiences of delivering digital first-line treatment for hip and knee osteoarthritis. Physiother Theory Pract. 2025;41 (5): 998-1007. doi: 10.1080/09593985.2024.2380478.
Fernandes LG, Devan H, Williams CM. At my own space, pace and place: a systematic review of qualitative studies of enablers and barriers to telehealth interventions for people with chronic pain. Pain. 2022; 163 (2): e165-e181. doi: 10.1097/j.pain.0000000000002364.
Fraser C, Beasley M, Macfarlane G, Lovell K. Telephone cognitive behavioural therapy to prevent the development of chronic widespread pain: a qualitative study of patient perspectives and treatment acceptability. BMC Musculoskelet Disord. 2019; 20 (1):198-1008. doi: 10.1186/s12891-019-2584-2.
Koppenaal T, Pisters MF, Kloek CJ, Arensman RM, Ostelo RW, Veenhof C. the 3-month effectiveness of a stratified blended physiotherapy intervention in patients with nonspecific low back pain: cluster randomized controlled trial. J Med Internet Res. 2022; 24 (2): e31675. doi: 10.2196/31675.
Lawford BJ, Delany C, Bennell KL, Hinman RS. "I was really sceptical...But it worked really well": a qualitative study of patient perceptions of telephone-delivered exercise therapy by physiotherapists for people with knee osteoarthritis. Osteoarthritis Cartilage. 2018; 26 (6):741-750. doi: 10.1016/j.joca.2018.02.909.
Seron P, Oliveros MJ, Gutierrez-Arias R, Fuentes-Aspe R, Torres-Castro RC, Merino-Osorio C, et al. Effectiveness of telerehabilitation in physical therapy: a rapid overview. Phys Ther. 2021; 101 (6): 1-18. doi: 10.1093/ptj/pzab053.
Why You Should Consider Virtual Athletic Therapy
When people hear “virtual rehab”, they often think it must be less effective because it’s not hands-on. But the evidence shows otherwise.
When people hear “virtual rehab”, they often think it must be less effective because it’s not hands-on. But the evidence shows otherwise.
While telehealth has been growing since before 2020, the COVID-19 pandemic certainly accelerated its adoption— and the research to support it. We now have a much clearer picture of how virtual rehabilitation performs, and the evidence shows it is a strong, effective alternative to in-person musculoskeletal rehab.
Overall, the research shows that telehealth is just as effective as traditional in-person appointments for improving pain and physical function, with patients reporting overall satisfaction and positive experiences. Several recurring themes help explain these results and make telehealth a genuinely modern way to deliver rehabilitation.
Ease, Flexibility, and Convenience
One of the major benefits of virtual care is the convenience of appointments and the scheduling flexibility, removing some of the practical barriers to injury rehab. Online appointments eliminate the need to drive to and from a physical location and sit in a waiting room, taking away more time from your day. Appointments can be met wherever you are, and offer flexibility and efficiency in terms of your pace, your space, and your time. This is a benefit for those with hectic schedules, live in more rural areas, or who need quick access to a professional.
More Comfort at Home
To add to that, many patients reported feeling more at ease at home, noting it as a “safe zone”, as opposed to sharing a space with other people, adding distractions. Patients felt they could be more open because of the comfort and privacy of being at home. As well, there is the added benefit of tailoring exercise programs to the space and equipment available at home.
Less Distraction, More Personal
To piggyback on patients feeling like they can open up more at home, this offers the opportunity for more personal communication with the therapist. Distractions of noises, interruptions, and others in the background are removed, leading to more meaningful and connected conversations. This is important because therapeutic alliance (the patient and therapist working together) has consistently been shown to be an important factor in people’s recovery from pain and injury. Patients have noted that the care they received felt more personalized and tailored to their own environment. Collaboration, warmth, and support between a patient and therapist can still exist without face-to-face contact.
More Focus on What Matters
Two more important factors for patients’ recovery are education and reassurance, which are commonly first-line treatments for those with pain and injury (especially low back pain). This is easily deliverable through virtual means, especially when there is that strong therapeutic alliance. Because of the distance between the patient and therapist, patients are left with self-management tools to guide their recovery, making them more active in the process. There is more onus on the patient to take control of their pain/injury as opposed to having a therapist there to apply a modality or massage an area.
Similar Experience from Providers
Aside from a few specific cases, virtual assessments are just as reliable as in-person ones for most common injuries and pain conditions. Detailed history-taking often becomes more effective in this relaxed setting, and functional or orthopedic tests can easily be adapted for video. Therapists can still accurately identify issues and create tailored, progressive plans with confidence.
Virtual athletic therapy provides the same high-quality outcomes and satisfaction as in-person sessions — with added benefits like convenience, flexibility, time efficiency, and comfort. It’s an effective, evidence-backed option for anyone looking to assess, understand, and rehabilitate their sports or activity-related injuries, no matter where they are.
References:
Barton, C. J., Ezzat, A. M., Merolli, M., Williams, C. M., Haines, T., Mehta, N., et al. “It's second best”: A mixed-methods evaluation of the experiences and attitudes of people with musculoskeletal pain towards physiotherapist delivered telehealth during the COVID-19 pandemic. Musculoskeletal Science and Practice. 2022; 58, Article 102500. https://doi.org/10.1016/j.msksp.2021.102500.
Bennell KL, Marshall CJ, Dobson F, Kasza J, Lonsdale C, Hinman RS. Does a web-based exercise programming system improve home exercise adherence for people with musculoskeletal conditions?: A randomized controlled trial. Am J Phys Med Rehabil. 2019; 98 (10): 850-858. doi: 10.1097/PHM.0000000000001204.
Bucki FM, Clay MB, Tobiczyk H, Green BN. Scoping review of telehealth for musculoskeletal disorders: applications for the COVID-19 pandemic. J Manipulative Physiol Ther. 2021; 44 (7): 558-565. doi: 10.1016/j.jmpt.2021.12.003.
Cottrell MA, Galea OA, O’Leary SP, Hill AJ, Russell TG. Real-time telerehabilitation for the treatment of musculoskeletal conditions is effective and comparable to standard practice: a systematic review and meta-analysis. Clin Rehab. 2017; 31 (5): 625-638. doi: 10.1177/0269215516645148.
Cottrell MA, O’Leary SP, Raymer M, Hill AJ, Comans T, Russell TG. Does telerehabilitation result in inferior clinical outcomes compared with in-person care for the management of chronic MSK spinal conditions in the tertiary hospital setting? J Telemed Telecare. 2021; 27 (7): 444-452. doi: 10.1177/1357633X19887265.
Cottrell MA, Russell TG. Telehealth for musculoskeletal physiotherapy. Musculoskelet Sci Pract. 2020 ;48: Article 102193. doi: 10.1016/j.msksp.2020.102193.
Cronström A, Sjödahl Hammarlund C. "A feeling of being part of the future": a qualitative study on physical therapists' experiences of delivering digital first-line treatment for hip and knee osteoarthritis. Physiother Theory Pract. 2025;41 (5): 998-1007. doi: 10.1080/09593985.2024.2380478.
Fernandes LG, Devan H, Williams CM. At my own space, pace and place: a systematic review of qualitative studies of enablers and barriers to telehealth interventions for people with chronic pain. Pain. 2022; 163 (2): e165-e181. doi: 10.1097/j.pain.0000000000002364.
Fraser C, Beasley M, Macfarlane G, Lovell K. Telephone cognitive behavioural therapy to prevent the development of chronic widespread pain: a qualitative study of patient perspectives and treatment acceptability. BMC Musculoskelet Disord. 2019; 20 (1):198-1008. doi: 10.1186/s12891-019-2584-2.
Koppenaal T, Pisters MF, Kloek CJ, Arensman RM, Ostelo RW, Veenhof C. the 3-month effectiveness of a stratified blended physiotherapy intervention in patients with nonspecific low back pain: cluster randomized controlled trial. J Med Internet Res. 2022; 24 (2): e31675. doi: 10.2196/31675.
Lawford BJ, Delany C, Bennell KL, Hinman RS. "I was really sceptical...But it worked really well": a qualitative study of patient perceptions of telephone-delivered exercise therapy by physiotherapists for people with knee osteoarthritis. Osteoarthritis Cartilage. 2018; 26 (6):741-750. doi: 10.1016/j.joca.2018.02.909.
Seron P, Oliveros MJ, Gutierrez-Arias R, Fuentes-Aspe R, Torres-Castro RC, Merino-Osorio C, et al. Effectiveness of telerehabilitation in physical therapy: a rapid overview. Phys Ther. 2021; 101 (6): 1-18. doi: 10.1093/ptj/pzab053.
Who Am I As an Athletic Therapist?
Athletic therapy isn’t just my job; it’s something I've been immersed in since starting school in 2013 and becoming certified in Canada in 2017. Here’s a look at my experience, education, and the principles that guide how I work with people.
Athletic therapy isn’t just my job; it’s something I've been immersed in since starting school in 2013 and becoming certified in Canada in 2017. Here’s a look at my experience, education, and the principles that guide how I work with people.
Placements were an integral part of Sheridan College’s athletic therapy program, with mornings in class and afternoons in the field working with college and university sports teams. Centennial College offered me a variety of experiences with the women’s soccer, men’s volleyball, and badminton teams. Much to my surprise, it was the badminton team I enjoyed the most— they’d never had a dedicated student therapist before, so they certainly made the most of having one. At this stage, I was still a newbie, but my next placement with Ontario Tech University’s women’s hockey team was where I really started to hit my stride. I had become more confident in my assessments and clinical rehab, and I felt part of the team. I particularly enjoyed the rush of pre-game preparation with the excitement and anticipation of the game.
By far, though, the best and most memorable school placement was with the Toronto Blue Jays in 2016— the deciding factor in choosing Sheridan’s program, since other schools did not offer this. It was a crash course in what life in professional sports is really like. At times, it felt surreal being in the same room with the players I watched on TV, or telling people I was in the clubhouse for all 81 home games. But it was also an invaluable look into the high standards and daily demands of pro athletes. It confirmed that the professional sports lifestyle was not for me, but I still wanted to be involved in baseball, and it helped shape how I practice today.
Just two months after becoming certified, I started working with Baseball Canada’s Junior National Team for the WBSC U18 Baseball World Cup. It was a long three weeks of training camp and competition, which resulted in a loss in the bronze medal game, but it was the start of six years with the program. I’ve been fortunate enough to follow many of those players through their careers, several of whom are now in the MLB. My involvement in baseball expanded from there: organizing athletic therapy field coverage for Baseball Canada’s 2019 U15 Ray Carter Cup, providing field coverage for the Toronto Blue Jays Baseball Academy Canadian Futures Showcase, and covering a couple of training sessions for Softball Canada’s Women’s National Team.
Since 2018, most of my day-to-day work has been in the clinic— a different world from dugouts and benches. Here, it is about understanding someone’s pain problem and building a progressive plan around their goals, capacity, and desired activities. This balance of acute care on-field and clinical rehab has given me a full view of the injury and rehab process— a unique perspective that athletic therapy brings.
My formal education in athletic therapy, which I supplemented with becoming a registered massage therapist, laid the foundation, but it has been a combination of working with patients and ongoing learning that has shaped how I practice today. Naturally drawn to baseball and shoulder injuries, Jared Powell’s three-part shoulder course deepened my understanding of how to assess and manage the many variations of shoulder pain. But the most influential courses I’ve taken were Greg Lehman’s Reconciling Biomechanics with Pain Science and Running Resiliency courses. These courses take a more broad approach to understanding assessment and rehab and have really helped me reflect on these aspects of my profession. I also like to stay on top of current best practices by reading a variety of research and journal articles.
Through all of my experience and education, a few principles have stayed constant:
1) The body is not fragile nor broken, but rather adaptable when the loads are appropriate.
2) Rehab should be active rather than passive; the right loads drive change, and engaged patients recover better.
3) Education is key— understanding your injury gives you the confidence and control to move forward.
What this means for you is whether you’re an athlete, physically active on your own, or just someone who wants to move without pain holding you back. My approach is grounded in over eight years of experience across every level of sport, combined with a commitment to evidence-based rehab to help you build resilience and confidence in your activity.
Why an Athletic Therapist Should Be Your Go-to For Your Sports Injuries
From the moment an injury happens on the field to the final stage of your recovery, athletic therapists are trained to manage the whole journey.
Injuries are never fun, but they are unfortunately a fact of life. Choosing the right professional can mean the difference between bouncing back fully, or dealing with an injury that keeps bouncing back. One profession you may not have heard of - but should know about - is athletic therapy.
Athletic therapy grew from the world of sports and has been dealing with athletic injuries for a long time. You have probably seen athletic therapists without knowing it— if you’re ever watching a sport like rugby or hurling and you see a member of the team staff run out to attend to an injured player, there’s a good chance that is an athletic therapist. This is because athletic therapists have extensive and ongoing training in the assessment of on-field acute injuries, but also in emergency care, including concussion assessment. Athletic therapists are trained to quickly sport whether an injury is serious and decide if it is safe to keep playing. Athletic therapists can be found at all levels of sport, from youth leagues all the way up to the professional and international level, ensuring participants stay safe. They are an integral part of the team because of this ability to assess and manage injuries right when they occur, setting the stage for recovery right from the get-go.
Athletic therapists also have extensive training in injury rehabilitation. This is more of a clinical setting where the athletic therapist takes their time to fully assess an injury or pain you have been dealing with, and then provides a treatment plan to help you get better. Because athletic therapists deal with active individuals and those who play sports, we know what the demands of sports are and therefore the rehab needs to be a little more than what you might think of with typical rehab. This is because the goal is to get you back to your sport or activity— the rehab needs to prepare you for this return. As such, athletic therapists don’t just focus on easing pain— it’s about building the strength, control, and confidence you need to get back to your sport and stay there.
From the moment an injury happens on the field to the final stage of your recovery, athletic therapists are trained to manage the whole journey.
This shouldn’t intimidate you though, if you feel you are not active enough or not a high-level athlete to see an athletic therapist. Athletic therapy really is for anyone who moves and wants a rehab approach that respects that. Athletic therapy takes an active approach to sports injury rehab because movement and exercise are what prepares you for that return to sports with more resilience and the confidence to participate without fear of reinjury.
Athletic therapy is a trusted part of the sports medicine world, but more importantly it is built around helping people recover and return to their sports. They are woven into the sports and activity community, from the sideline to the clinic, helping people recover stronger and get back to what they love. If you’re active, dealing with pain, or just want to move with more confidence, athletic therapy is built for you.
The Story Behind the Name
Bend Without Breaking – the ability to adapt, respond, spring back and grow stronger in the face of challenges or adversity, embodying strength, flexibility and persistence; a balance of toughness and resilience - like a branch that sways in the wind but does not snap.
Coming up with a name for my virtual athletic therapy services was a long and challenging process with lots of brainstorming and revisions. I wanted a name that not only would I be proud of, but would also reflect my philosophy and approach to rehabbing sports-related injuries. After testing out several names and thinking I had finally found the one, I kept coming back to Bend Without Breaking for the literal and figurative message behind the name.
Literally: many people who have experienced an injury or are dealing with pain in their daily lives often come out of their first appointment feeling like they are broken. They’re often told of all of these different mechanical or movement-based reasons for why they are in pain, such as their posture or how they run. They are then given all of these “diagnoses” followed by exercises to try and correct these issues. This leaves many people feeling that there is something wrong with them, that they have to change how they move, or they won’t get better. This is especially true when it comes to those with low back pain where they become afraid of bending their back or else they will make things worse. While we do know that certain movements and positions can be painful, this doesn’t mean that we’re broken or making things worse. Often times, we just need strategies to help manage pain, let things calm down, and then slowly build ourselves back up. Even with an injury, we are allowed to move, and it is often needed to help facilitate recovery.
Figuratively: we are adaptable human beings. When we expose ourselves to the right amount of stress, say when we work out in the gym, our body responds by getting stronger. If we continue to do this, our bodies become more and more resilient to the stresses we place upon ourselves, making us better able to tolerate all kinds of loads. This is ultimately what influences injury— the balance between the stress we place upon ourselves and our ability to tolerate that stress. If we can build for ourselves a larger window or capacity to tolerate stress, we’re less likely to get injured, even when we do push ourselves a little more.
Bend Without Breaking – the ability to adapt, respond, spring back and grow stronger in the face of challenges or adversity, embodying strength, flexibility and persistence; a balance of toughness and resilience - like a branch that sways in the wind but does not snap.
My main goal is to teach people that they are not broken, but rather unique individuals with the ability to adapt and spring back from an injury; to build resilience and confidence in themselves to continue with the activities they enjoy. The image that kept coming back into my mind when I think about my treatment approach was that tree branch swaying in the gust of wind, bending to the stress of the wind and not breaking, but rather returning back to its resting position when the wind stops.